APPENDICITIS CASE
Fatimah B. is a 20 year old female with severe abdominal pain since yesterday
History elements (these also indicate the questions that should be asked)
- The pain began in periumbilical region and moved towards right lower quadrant
- Pain is intermittent and achy in nature
- No aggravating or alleviating factors
- Currently pain is 6/10; at its worse the pain is 9/10
- Woke up with a fever of 100.4 F this morning
- In addition to pain, patient has been experiencing nausea and vomiting
- Vomit is clear, non-bloody, nonbilious
- Has had 2 episodes of vomiting
- Patient had one episode of non-bloody diarrhea this morning
- Has not eaten any new foods since yesterday
- Took OTC medications (tylenol) with no improvement
- Patient is not sexually active
- The patient does not have an OB/GYN and has never had a pap smear
- Denies hematuria, dysuria
- Denies vaginal bleeding/vaginal discharge
- Denies recent travel or sick contacts
- Her last menstrual period was two weeks ago
- She has never had children
- Denies chills, body aches, headache
Physical Exam (also indicates what procedures should be done)
- Vital signs – P89, BP 102/66, R 16, T 100.2 F
- Gen – patient is alert, in no acute distress, well-developed, well-nourished
- Abd – bowel sounds normoactive in all four quadrants with no aortic/renal/iliac or femoral bruits. Abdomen is soft, flat, positive RLQ tenderness, + McBurney’s point tenderness, non-distended, no guarding or rigidity, no masses palpable, no Rovsing sign. Negative CVA tenderness
- Pelvic- normally developed genitalia with no external lesions or eruptions. Vagina and cervix show no lesions, inflammation, discharge or tenderness. No cystoceles.
- Should order Urine Pregnancy Test, Urinalysis, Urine Culture, CBC w/ diff, abdominal ultrasound, abdominal CT scan, FOBT
Differential Diagnosis
- Appendicitis
- The presentation of the patient’s pain is highly characteristic of appendicitis. The pattern in which the pain migrates from the periumbilical region to the right lower quadrant is indicative of appendicitis. Additionally, the patient has a positive McBurney’s point which also indicates appendicitis.
- Gastroenteritis
- Since the patient has been experiencing abdominal pain with nausea and 2 episodes of non-bloody, non-bilious vomiting, the patient could very well have a case of viral gastroenteritis. This is typically diagnosed based on symptoms and physical exam.
- Ruptured ovarian cyst
- When a female is experiencing lower abdominal problems, it is important not to rule out possible gynecological causes! A ruptured ovarian cyst can cause sudden and severe abdominal pain, fever or vomiting, weakness, etc.– very similar symptoms that the patient was experiencing.
Tests (Student will be given results for any that are ordered):
- Urine Pregnancy Test: Negative
- Urinalysis
- Leukocyte esterase: 75
- Nitrites: neg
- Urobilinogen: normal
- Protein: negative
- pH: 6
- Blood: neg
- Specific gravity: 1.020
- Ketones: neg
- Bilirubin: neg
- Glucose: neg
- Complete Urinalysis:
- Yeast: present
- Color: yellow
- Appearance: Turbid
- pH: 5.5
- Specific gravity: 1.027
- Glucose: neg
- Protein: trace
- Ketone: trace
- Blood: neg
- Urobilinogen: <2
- WBC: 5-10 (H)
- RBC: 0-2
- Bacteria: trace
- Epithelial cells: none
- Leukocyte esterase: trace
- Nitrite: neg
- Hyaline casts: trace
- Bilirubin: neg
- Urine Culture: no growth
- FOBT: negative
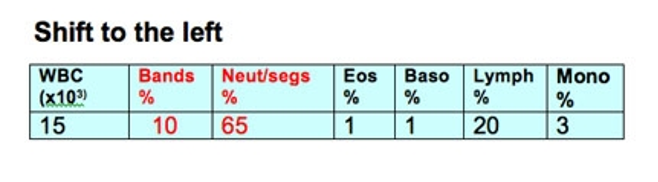
- CBC:
- WBC: 15,000 mm^3
- Hb:13.0
- HCT:40%
- Plt: 200,000/mm^3
- Abdominal Ultrasound
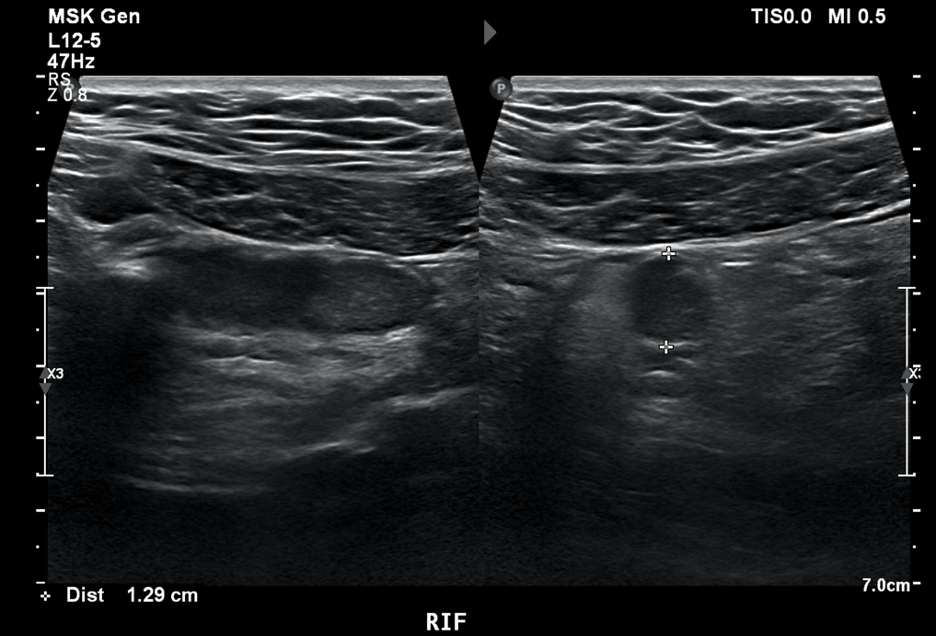
- There is blind-ending, non-compressible tubular structure seen at the right iliac fossa representing the enlarged vermiform appendix. It was tender on probing
- There is an echogenic structure seen at the base of the appendix associated with acoustic shadowing representing an appendicolith
- There is increased echogenicity of the fat surrounding the appendix
- The lumen of the appendix is distended with diffuse internal echoes that could represent the accumulation of secretion/mucin or pus

- This image shows a dilated, thick-walled appendix (arrows) with surrounding inflammatory changes
Treatment
- Supportive treatment!
- NPO
- IV fluids
- Electrolyte repletion as needed
- IV analgesics
- IV antiemetics as needed (Zofran)
- Antipyretic therapy
- Treat patient with preoperative antibiotics for uncomplicated appendicitis
- Cefoxetin 1-2 g IV q 6hrs (can be stopped after surgery)
- Appendectomy within 24 hours of diagnosis is the current standard of care for acute uncomplicated appendicitis (laparoscopic or open appendectomy)
Pt. counseling
- Patient must monitor the incision site for any signs of infection such as redness, swelling, drainage, or increased pain and report these to their surgeon
- Staples or sutures will be removed in 5-7 days; they must follow up with surgeon or primary provider for wound check and assessment
- Normal activity can resume within a few days to a week however, strenuous activity should be avoided for the first 4-6 weeks
- Patient must complete course of antibiotics and take with meal should stomach upset occur
- If patient is prescribed pain meds such as opioids, will instruct patient to not drive or operate machinery, and to take a stool softener to avoid constipation
- Encourage patient to bring any unexpected findings to their provider


